Abstract
Background: Multiple myeloma is a plasma cell malignancy. With the emerging novel therapy and deepening response to therapy, minimal residual disease (MRD) now has been widely accepted as the response assessment beyond complete response. New generation flow (NGF) and new generation sequencing (NGS) assess the MRD status of the bone marrow, which might result in false-negative MRD because of the well-known spatially heterogeneous and extramedullary involvement in MM. To overcome this limitations, whole body functional imaging technique such as positron emission tomography/computed tomography (PET/CT) is required. To our knowledge, there is limited data examining the prognostic value of flow MRD and FDG-PET/CT at multiple time points before and after ASCT in MM. In this study, we aimed to elucidate the prognostic valued of MRD by flow combined with PET/CT at different time points in the long-term outcomes for transplant-eligible NDMM patients.
Methods: This observational cohort study was approved by the ethnic committee of Sun Yat-sen University. The inclusion criteria were 1) patients with transplant eligible NDMM; 2) received uniform induction regimen of PAD and proceeded to the following ASCT; 3) received PET/CT scan in our hospital before receiving any anti-myeloma therapy. Whole-body 18F-FDG PET/CT was carried out in all patients at baseline and was then repeated post-induction (median 38days after the completion of induction), and at 6th, 12th and 24th month post-transplant. Flow MRD status were analyzed by 8-color multiparameter flow cytometry with the sensitivity of 10 -5.
Results:
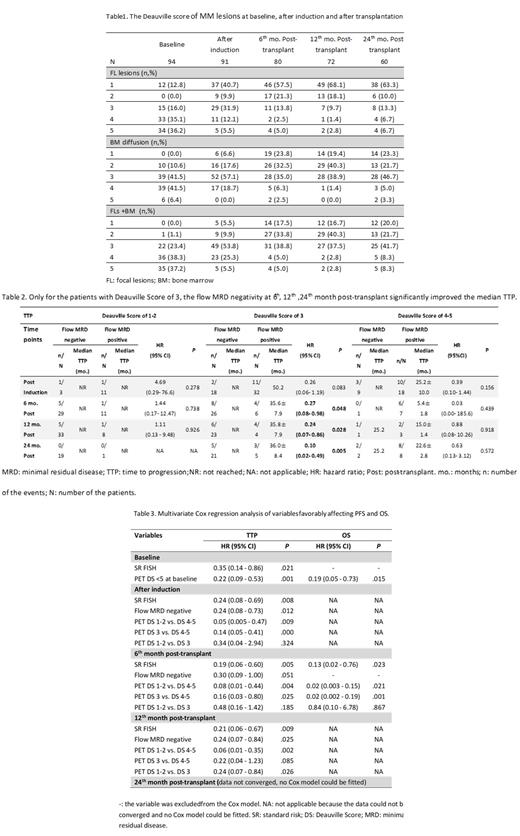
From July 2012 to Apr 2017, 94 consecutive patients with transplant eligible NDMM were included in the final analysis. To standardize the PET/CT interpretation, 5-points scale of Deauville score (DS) was applied to evaluate the FDG uptake of bone marrow and focal lesions together.
"Flow MRD" and "PET Deauville score" were highly discordant. No matter choosing DS 1, 2 or 3 as the cutoff for PET/CT positivity, there was no significant agreement between PET/CT and flow MRD assessment after induction. At 6th and 12th month post-transplant, neither existed the significant agreement between these 2 assessments if DS 1 or 2 as the cutoff; even if DS 3 as the cutoff, the agreement degree was very poor at these early time points post-transplant. At the 24th month post-transplant, adopting DS3 as the cutoff for PET/CT positivity, the agreement degree between flow MRD and PET/CT was significantly improved to moderate level with the kappa score of 0.579.
In the univariate analysis, no matter the flow MRD status was positive or negative, patients with PET DS1-2 at each time points had similar favorable TTP (table 2) whereas patients with PET DS4-5 at each time points had similar poor TTP. In the subgroup of PET DS3, as early as after the induction, patients with flow MRD-negative already show the trend of better TTP (p = .083); while at the 6th, 12th, 24th month post-transplant, patients with flow MRD - negative had significantly better TTP than those with flow MRD - positive.
In the multivariate analysis (table3), the lesion DS≤4 at baseline and standard risk FISH were Independent predictive factors for TTP and the lesion DS ≤4 was the only independent predictive factor for OS. After induction and 6th month after transplant, the baseline DS were excluded from the Cox model. The post-therapy PET DS 3 might be a good cutoff value for PET/CT MRD positivity because it significantly predicted both the TTP and OS. However, since 12th month after transplant, compared to patients with DS3, those with DS 1-2 had favorably TTP. The cutoff value shifted to DS2.
Conclusion: PET/CT and flow MRD are highly discordant until 2 years after transplant for patients with NDMM. Patients with low Deauville score (1-2) had good prognosis at different time points no matter the MRD status, reflecting the importance of PET/CT in evaluation the aggressive degree of MRD clone. Patients with high Deauville score (4-5) had poor prognosis at different time points no matter the MRD status, reflecting the importance of PET/CT in overcoming the uneven and extramedullary disease in MM. The Deauville score of PET/CT remained as the independent prognosis factor at post-induction, 6 th -, 12 th -, and 24 th month post-transplant. However, the cut-off value of PET/CT Deauville score shift from score 3 before 1-year post-transplant to score 2 at and beyond 1-year post-transplant.
No relevant conflicts of interest to declare.